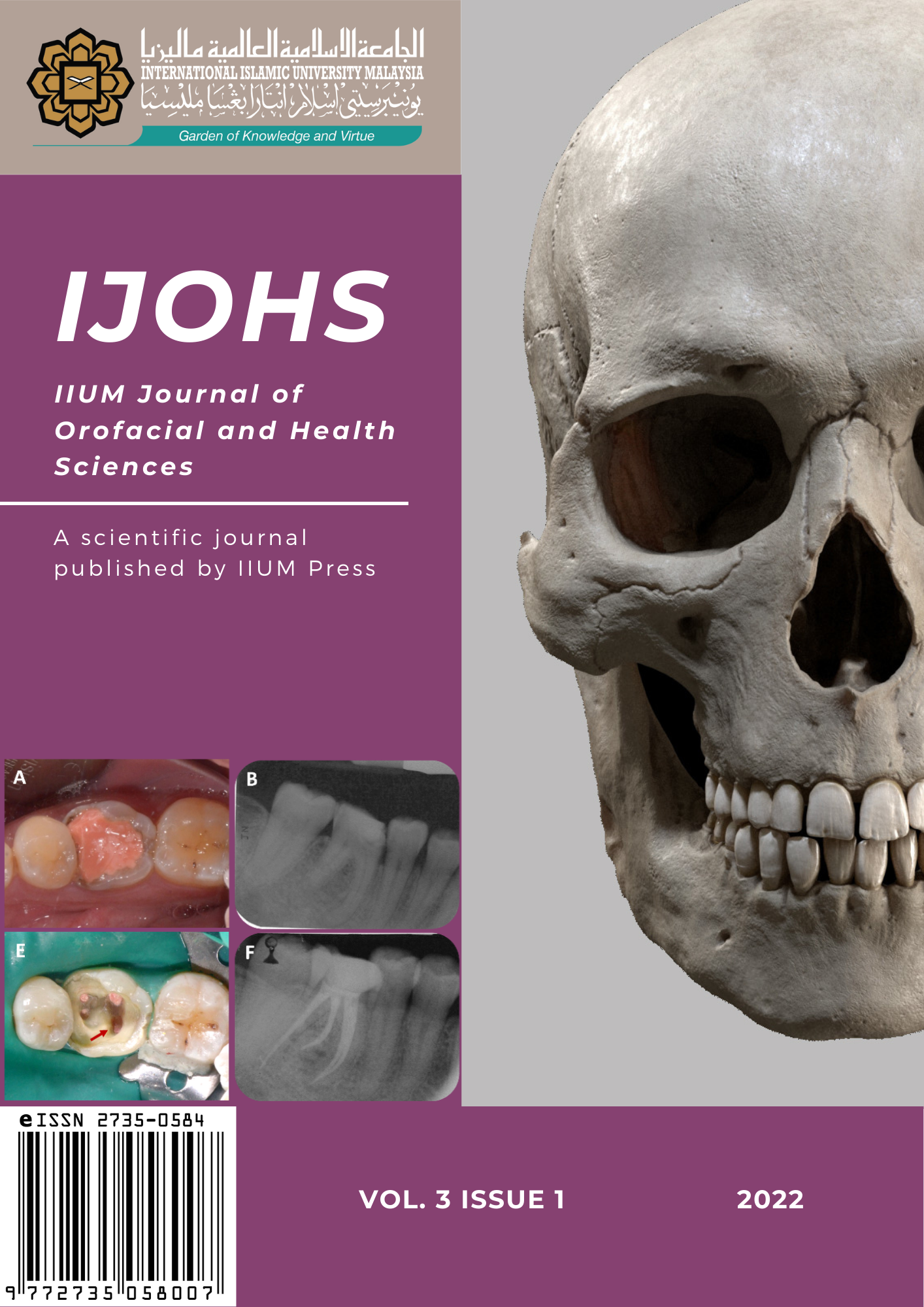
Minor oral surgery on impacted lower third molar done by IIUM Undergraduates: a retrospective study
DOI:
https://doi.org/10.31436/ijohs.v3i1.103Keywords:
impacted tooth, minor oral surgery, difficulty level, wisdom tooth, third molarAbstract
Minor oral surgery (MOS) is one of the important requirements for dental undergraduates to perform in Kulliyyah of Dentistry, IIUM. However, no assessment has been done on the suitability of the cases received by the students. Thus, this study was aimed to describe type of cases and level of difficulty in relation to undergraduate year of study. This study consisted of 97 subjects who had undergone MOS by IIUM undergraduate from September 2014 to October 2015. Data was collected from patient’s documentation and orthopantomogram. Pederson index and relationship to inferior dental nerve were used to determine the difficulty index level. Statistical analysis was done using Chi-square test with statistical significance set at p? 0.05. The mean age of the patients was 24 years old, with male to female ratio 1:1.9. 52.6% of the cases were indicated for surgery due to recurrent pericoronitis. The types of cases mostly received by undergraduates were Class IA (30.9%) and Class IIA (48.5%) with mesioangular impaction (39.2%). Year 4 students received more difficult cases compared to Year 5 (p = 0.504) with less complications postoperatively. Dental undergraduates received simple to moderate cases for MOS, and no significant association was found between year of undergraduate study and difficulty level of the cases.
References
Abdulai, A.E., Nuamah, I.K., Sackeyfio, J., & Hewlett, S. (2014). Indications for surgical extraction of third molars: a hospital-base study in Accra, Ghana. International Journal of Medicine and Biomedical Research, 3(3), 155–160.
Al-Anqudi, S.M., Al-Sudairy, S., Al-Hosni, A., & Al-Maniri, A. (2014). Prevalence and pattern of third molar impaction: A retrospective study of radiographs in Oman. Sultan Qaboos University Medical Journal, 14(3), 388–392.
Ali, K., McCarthy, A., Robbins, J., Heffernan, E., & Coombes, L. (2014). Management of impacted wisdom teeth: teaching of undergraduate students in UK dental schools. European Journal of Dental Education, 18(3), 135–141.
Bali, A., Bali, D., Sharma, A., & Verma, G. (2012). Is Pederson Index a true predictive difficulty index for impacted mandibular third molar surgery? A meta-analysis. Journal of Maxillofacial and Oral Surgery, 12(3), 359–364.
Bataineh A.B. (2001). Sensory nerve impairment following mandibular third molar surgery. Journal of Oral and Maxillofacial Surgery, 59(9), 1012–1017.
Batal, H.S., & Jacobs, G. (2006). Surgical Extractions. In: Koerner K. R. (ed.), Manual of Minor Oral Surgery for The General Dentist (1st ed.). London: Blackwell Munksgaard, pp. 19–48.
Blaeser, B.F., August, M.A., Donoff, R.B., Kaban, L.B., & Dodson, T.B. (2003). Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. Journal of Oral and Maxillofacial Surgery, 61(4), 417–421.
Bui, C.H., Seldin, E.B., & Dodson, T.B. (2003). Types, frequencies, and risk factors for complications after third molar extraction. Journal of Oral and Maxillofacial Surgery, 61(12), 1379–1389.
Byahatti, S., & Ingafou, M.S. (2012). Prevalence of eruption status of third molars in Libyan students. Dental Research Journal, 9(2), 152–157.
Evans, A.W., Aghabeigi, B., Leeson, R.M., O'Sullivan, C., & Eliahoo, J. (2002). Assessment of surgeon competency to remove mandibular third molar teeth. International Journal of Oral and Maxillofacial Surgery, 31(4), 434–438.
Fuselier, J.C., Ellis, E.E., 3rd, & Dodson, T.B. (2002). Do mandibular third molars alter the risk of angle fracture? Journal of Oral and Maxillofacial Surgery, 60(5), 514–518.
Gülicher, D., & Gerlach, K. (2001). Sensory impairment of the lingual and inferior alveolar nerves following removal of impacted mandibular third molars. International Journal of Oral and Maxillofacial Surgery, 30(4), 306–312.
Halmos, D.R., Ellis, E., 3rd, & Dodson, T.B. (2004). Mandibular third molars and angle fractures. Journal of Oral and Maxillofacial Surgery, 62(9), 1076–1081.
Hassan A.H. (2010). Pattern of third molar impaction in a Saudi population. Clinical, Cosmetic and Investigational Dentistry, 2, 109–113.
Haug, R.H., Perrott, D.H., Gonzalez, M.L., & Talwar, R.M. (2005). The American Association of Oral and Maxillofacial Surgeons age-related third molar study. Journal of Oral and Maxillofacial Surgery, 63(8), 1106–1114.
Hill, C., Mostafa, P., Thomas, D., Newcombe, R., & Walker, R. (2001). Nerve morbidity following wisdom tooth removal under local and general anaesthesia. British Journal of Oral and Maxillofacial Surgery, 39(6), 419–422.
Hupp, J.R. (2014). Principles of Management of Impacted Teeth. In: Ellis, E. E. 3rd, Tucker, M. R. (eds.), Contemporary Oral and Maxillofacial Surgery (6th ed.). Missouri: Elsevier Mosby, pp. 143-147.
Krimmel, M., & Reinert, S. (2000). Mandibular fracture after third molar removal. Journal of Oral and Maxillofacial Surgery, 58(10), 1110–1112.
Ma’aita J.K. (2000). Impacted third molars and associated pathology in Jordanian patients. Saudi Dental Journal, 12, 16–19.
Malik, N.A. (2012). Minor Oral Surgical Procedures. In: Malik, N. A. (ed.), Textbook of Oral and Maxillofacial Surgery (3rd ed.). New Delhi: Jaypee Brothers Medical Publisher, pp. 147.
Mehrabi, M., Allen, J.M., & Roser, S.M. (2007). Therapeutic agents in perioperative third molar surgical procedures. Oral and Maxillofacial Surgery Clinics of North America, 19(1), 69–84.
Merry, A., Gibbs, R., Edwards, J., Ting, G., Frampton, C., Davies, E., et al., (2010). Combined acetaminophen and ibuprofen for pain relief after oral surgery in adults: a randomized controlled trial. British Journal of Anaesthesia, 104(1), 80–88.
Ministry of Health Malaysia (2005). Clinical Practice Guidelines: Management of Unerupted and Impacted Third Molar Teeth. Retrieved 8 January 2015, from https://www.moh.gov.my/moh/attachments/3931.pdf
Ministry of Health Malaysia (2015). Clinical Practice Guidelines: Antibiotic Prophylaxis in Oral Surgery for Prevention of Surgical Site Infection. Retrieved 8 March 2021, from https://www.moh.gov.my/moh/resources/Penerbitan/CPG/Dental%20&%20Oral/CPG_Antibiotic_Prophylaxis_in_Oral_Surgery_Nov_2015.pdf
National Institute for Health & Care Excellence (2000). Guidance on the Extraction of Wisdom Teeth. Retrieved 23 December 2015, from https://www.nice.org.uk/guidance/ta1/chapter/1-guidance
Obiechina, A.E., Arotiba, J.T., & Fasola, A.O. (2001). Third molar impaction: evaluation of the symptoms and pattern of impaction of mandibular third molar teeth in Nigerians. Odonto-stomatologie Tropicale = Tropical Dental Journal, 24(93), 22–25.
Othman R. (2009). Impacted mandibular third molars among patients attending Hospital Universiti Sains Malaysia. Archives of Orofacial Sciences, 4, 7-12.
Quek, S.L., Tay, C.K., Tay, K.H., Toh, S.L., & Lim, K.C. (2003). Pattern of third molar impaction in a Singapore Chinese population: a retrospective radiographic survey. International Journal of Oral and Maxillofacial Surgery, 32(5), 548–552.
Shetty, P., & Banerjee, S. (2010). Missing molars: A study on status of third molars. Journal of Pharmaceutical and Biomedical Sciences, 4(4), 1-3.
Susarla, S. M., Blaeser, B. F., & Magalnick, D. (2003). Third molar surgery and associated complications. Oral and Maxillofacial Surgery Clinics of North America, 15(2), 177–18
Susarla, S. M., & Dodson, T. B. (2004). Risk factors for third molar extraction difficulty. Journal of Oral and Maxillofacial Surgery, 62(11), 1363–1371.
World Health Organization (2010). WHO Pain Ladder with Pain Management Guidelines. Retrieved 31 December 2015, from https://www.southwesthealthline.ca/healthlibrary_docs/B.5.3.WHOPainLadder.pdf
Yuasa, H., Kawai, T., & Sugiura, M. (2002). Classification of surgical difficulty in extracting impacted third molars. The British Journal of Oral & Maxillofacial Surgery, 40(1), 26–31.